Case Report / Open Access
DOI:10.31488/bjg.1000136
Evolution of Cutaneous Lesion Resulting from Non-Target Embolization of the Hepatic Falciform Artery: A Case Report
Olumide Olulade, Jalil Kalantari, Dmitry Rabkin*
1. Division of Angiography and Interventional Radiology, Department of Radiology, Brigham and Women’s Hospital, 75 Francis Street, Boston, MA 02115, USA
*Corresponding author: Dmitry Rabkin, MD, PhD, FSIR Department of Radiology,Brigham and Women’s Hospital
Abstract
Non-target embolization of the hepatic falciform artery is a rare complication of transcatheter arterial liver-directed therapy. The low prevalence of the falciform artery and the use of preparation angiographic mapping prior to treatment perhaps accounts for the relative paucity of reported cases. An indolent course is reported to accompany the associated cutaneous manifestations; however, a depiction of the timeline healing has not been shown to date and may be useful for providers when counseling patients in the event of occurrence of this complication. Here, we present a case of non-target embolization of the falciform artery following transarterial chemoembolization and provide pictorial representations of the cutaneous lesion and subsequent healing over the following months.
Keywords: Chemoembolization, falciform artery, non-target embolization, liver cancer
Background
Hepatic malignancies represent a significant cause of morbidity and mortality world-wide, with greater than 900,000 new cases and 800,000 related deaths reported in 2020 [1]. In patients with multifocal liver metastasis and/or poor hepatic functional reserve, treatment options such as liver transplantation, systemic chemotherapy, surgical resection, or ablative therapies [2] are undesirable and often impractical. In such cases, loco-regional treatment with transcatheter arterial chemoembolization (TACE) or radioembolization (TARE) is well-established, taking advantage of the fact that hepatic tumors primarily derive their blood supply from the hepatic artery, while the liver parenchyma derives its supply primarily from the portal vein. Complications of this procedure include hepatic and/or renal failure, ischemic cholecystitis, pancreatitis, and duodenal ulceration [3], often a result of non-target embolization. Less commonly, cutaneous manifestations arise from non-target embolization of the hepatic falciform artery [4], a vascular variant with prevalence reportedly as low as 2% [5]. Several studies have described these manifestations, which are known to be self-limiting. This however remains an unwanted complication, which can lead to much distress for patients, especially when unaware of the nature of the cutaneous injury, and expected time-course of healing. Here, we present a case of non- target falciform artery embolization, with pictorial representations of the cutaneous manifestations and subsequent healing process.
Case Report
The current case report was prepared under approved Dana Farber Cancer Institute Institutional Review Board protocol (DFCI #21-551) for retrospective analysis of clinical cases. The patient was a 53-year-old female diagnosed with metastatic ileal carcinoid tumor to the liver in 2014. Following initiation of monthly Octreotide, which provided symptomatic relief, it was determined that she would benefit from liver directed treatment. Following informed consent, it was decided to proceed with treatment.
Preparation mapping angiography was performed in October 2015, demonstrating expected tumor blush within both hepatic lobes on super selective angiography of the hepatic arteries. Prophylactic coil embolization of the gastroduodenal and right gastric arteries was performed based on imaging findings. Injection of Technetium-99m macro-aggregated albumin (99mTc-MAA) revealed a hepatopulmonary shunt ratio of 4.49%, within acceptable limits, and SPECT-CT demonstrated no extra- hepatic uptake. TARE of the right and left hepatic arteries was performed in November 2015 and December 2015 respectively. Both procedures were well-tolerated without post-procedural side effects. Good tumor response was observed based on subsequent imaging and improvement in patient’s symptoms.
Following stable restaging scans from 2016 to 2019, an increase in hepatic metastatic burden was noted on scans from September 2020, accompanied by worsening of symptoms. Repeat TACE with drug-eluting beads (DEB-TACE) of the right and left hepatic arteries was successfully performed in November 2020 and January 2021 respectively. Following the second treatment in January 2021, the patient contacted the Interventional Radiology team describing a mottling appearance of the mid abdomen, with linear pattern of bruising near the umbilicus that was first noticed the morning after the procedure (Figure 1a). This was accompanied by abdominal discomfort, amenable to mild analgesic therapy. The patient was counseled that the peri-umbilical bruising was likely related to inadvertent embolization of the hepatic falciform artery and assured that the cutaneous injury would resolve over time without specific intervention. Early spontaneous healing of the area of bruising was noted over the following week (Figure 1b-d), with the lesion shown to recede and coalesce during this period. Continued healing was noted over the subsequent months (Figure 1e). Within one year, there was complete healing of the lesion, without residual scarring (Figure 1f).
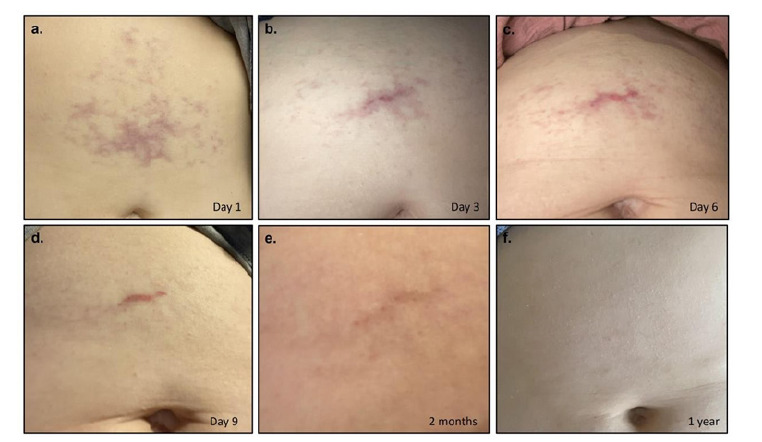
Figure 1.Mottled appearance of the mid abdomen with reticular pattern of periumbilical bruising noticed the morning after the procedure (a), consistent with inflammatory and ischemic skin changes from non-target hepatic falciform artery embolization. Immediate healing was noted over the next few days (b-d) and continued over the subsequent months (e). Within one year, there was complete resolution of the lesion, without any residual scarring (f).
Discussion
Potential complications of transcatheter arterial chemoembolization are well-documented [6], and often arise as a result of non-target embolization. Specifically, cutaneous complications can result from non-target embolization of the falciform artery [4,7]. Anatomically, this artery arises from the left or middle hepatic artery as a diminutive terminal branch that courses along the caudal aspect of the falciform ligament, and terminates within one of the layers of the anterior abdominal wall. Reports of falciform artery embolization describe a relatively indolent course, with symptoms of mild abdominal pain and peri-umbilical skin rash as seen in this case. As depicted in the figures, spontaneous healing may begin as early as one week, with complete healing potentially occurring within one year, without residual scarring. Mitigation of the associated pain with mild analgesics and complete resolution of pain within a few days was also reported in this case.
Despite the indolent course, this remains an unwanted complication, and several measures are undertaken to limit its likelihood of occurrence. Diagnostic angiography is routinely performed prior to liver-directed therapy to delineate the hepatic arterial anatomy. During this time, care is taken to identify the potential presence of a falciform artery. Notably, none was identified during preparation angiography prior to any of the treatments in this case, nor was cutaneous uptake noted on pre-treatment 99mTc-MAA single-photon emission computed tomography (SPECT/CT). Furthermore, no cutaneous complications were observed following the initial rounds of TARE and TACE. It is likely that over multiple treatments, with sequential embolization of the hepatic arteries, increasingly preferential flow to the falciform artery occurred, accounting for the presence of the complication only after the fourth overall treatment. Notably, cutaneous injury has also been seen as a result of non-target embolization of internal mammary and superior epigastric arteries.
If identified on preparatory angiography, prophylactic embolization of the falciform artery has been suggested prior to treatment [8], although no consensus exists regarding this. Application of ice packs to the anterior abdomen during the embolization procedure has been used to minimize the risks of non-target embolization, by promoting constriction of the falciform artery during embolic delivery [9]. Finally, intravenous administration of Dexrazoxane, an iron chelator used for cardioprotection against anthracyclines, has been demonstrated to prevent skin necrosis following non-target falciform artery embolization [10].
Conclusion
In summary, we present a case of non-target falciform artery embolization following liver- directed therapy with pictorial representations of the subsequent skin changes and healing, which began within one week, with no residual scarring observed after one year. We hope that this can be used as a reference tool for patients and providers when faced with this complication to demonstrate the potential expected changes, and the subsequent healing process.
Abbreviations
TACE: Transcatheter arterial chemoembolization; TARE: Transcatheter arterial radioembolization; 99mTc-MAA: Technetium-99m macro-aggregated albumin; DEB-TACE: Transcatheter arterial chemoembolization with drug-eluting beads (DEB-TACE); SPECT/CT: Single- photon emission computed tomography.
Conflicts of Interest
The authors declare that they have no competing interests. No funding support was received for this study.
Ethics Statement
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee, and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from the patient prior to each of the procedures described in this manuscript. Written informed consent for publication of their clinical details and/or clinical images was obtained from the patient.
References
1. Sung H, Ferlay J, Siegel RL, et al. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin. 2021;71(3):209-249.
2. Wáng YXJ, de Baere T, Idée JM, et al. Transcatheter embolization therapy in liver cancer: An update of clinical evidences. Chinese Journal of Cancer Research. 2015;27(2):96-121.
3. Riaz A, Lewandowski RJ, Kulik LM, et al. Complications Following Radioembolization with Yttrium-90 Microspheres: A Comprehensive Literature Review. J Vascular Interventional Radiol. 2009;20(9):1121-1130.
4. Bhalani SM, Lewandowski RJ. Radioembolization complicated by nontarget embolization to the falciform artery. Semin Intervent Radiol. 2011;28(2): 234-239.
5. Williams DM, Cho KJ, Ensminger WD, et al. Hepatic falciform artery: Anatomy, angiographic appearance, and clinical significance. Radiology. 1985;156(2): 339-340.
6. Leung DA, Goin JE, Sickles C, et al. Determinants of postembolization syndrome after hepatic chemoembolization. J Vasc Interventional Radiol. 2001;12(3): 321-326.
7. Leong QM, Lai HK, Lo RGH, et al. Radiation Dermatitis following Radioembolization for Hepatocellular Carcinoma: A Case for Prophylactic Embolization of a Patent Falciform Artery. J Vasc Interventional Radiol. 2009;20(6): 833-836.
8. Ueno K, Miyazono N, Inoue H, et al. Embolization of the hepatic falciform artery to prevent supraumbilical skin rash during transcatheter arterial chemoembolization for hepatocellular carcinoma. Cardiovasc Intervent Radiol. 1995;18(3): 183-185.
9. Wang DS, Louie JD, Kothary N, et al. Prophylactic topically applied ice to prevent cutaneous complications of nontarget chemoembolization and radioembolization. J Vasc Interventional Radiol. 2013;24(4): 596-600.
10. Stalder G, Deplanque G, Shabafrouz K, et al. Dexrazoxane prevents skin necrosis in non-target embolization of falciform artery during transcatheter arterial chemoembolization (TACE). Diagnostic and Interventional Imaging. 2018;99: 179- 180.
Received: January 06, 2023;
Accepted: February 15, 2023;
Published: February 17, 2023.
To cite this article : Olumide Olulade, Jalil Kalantari, Dmitry RabkinB. Evolution of Cutaneous Lesion Resulting from Non-Target Embolization of the Hepatic Falciform Artery: A Case Report. British Journal of Gastroenterology. 2023; 5(1): 278-280. doi: 10.31488/bjg.1000136
© Olulade O, et al. 2023.
