Case Report / Open Access
DOI:10.31488/bjg.1000131
Food Allergen Elimination for Adolescent Pre-diabetes Reduction
F. Buck Willis PhD, FACSM, Ronke Arogundade FNP, Elham Teimouri PhD, Nicole Maule MS,
1. Galveston ClinicalResearch, 6341 Stewart Rd #115, Galveston TX 77551, USA
*Corresponding author: F. Buck Willis PhD, FACSM Galveston ClinicalResearch, 6341 Stewart Rd #115, Galveston TX 77551, USA, Tel: 1-409-632-7131.
Abstract
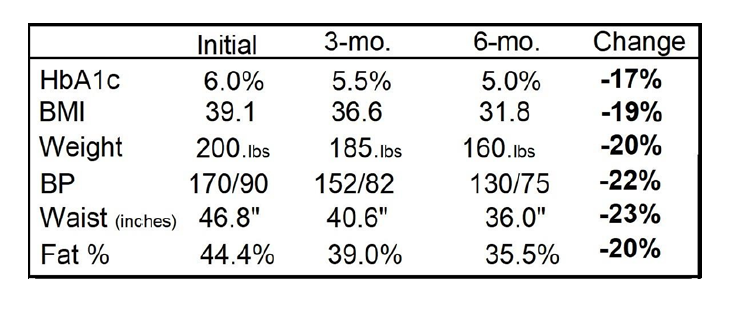
Today 24% of young adults in the USA have Pre-diabetes (HbA1c 5.7% - 6.4%), and Native Americans have twice the frequency of obtaining Type 2 Diabetes Mellitus (DM2) with a 50% greater chance of obesity. The purpose of this case report was to discuss changes following food allergen elimination in an obese patient with Pre-diabetes. Case: An 18-year-old female, Native American presented with HbA1c 6.0%, BMI = 39.1, Weight 200.lbs., BP 170/90, Waist 46.8”, and Fat = 44.4%. After consent was given, the patient was briefed on healthier eating (i.e. eliminate processed foods, high fructose corn syrup, etc.). Then thee vials of blood were drawn for ALCAT, Leukocyte Reaction, food allergen testing. Ten days later, the tests results were discussed, and of the 250 foods tested, the patient showed significant reactions to 33 foods. These foods were eliminated from her diet for the duration of this 6-month treatment plan and alternative food choices were discussed (i.e., eating almond butter instead of peanut butter which showed a significant Leukocyte reaction). She was also taught how to eat smaller positions (< 2 cups) more frequently (every 3-4 hours). The patient showed 98% compliance to the food allergen elimination. Results: All of the variables tested (HbA1c, BMI, Blood Pressure, Waist Circumference and Body Fat %) displayed meaningful reductions. (Table 1.) Food allergen elimination was an effective treatment method for reversing this adolescent Native American patient’s Pre-diabetes, and her HbA1c values went from 6.0% to 5.0% in six months without medication.
Background
Currently more than 35 million people in the United States have been diagnosed with Type II Diabetes Mellitus (DM2) and in 2017 this disease cost the United States over $325 billion dollars. Today, over 96 million adults in the USA have Pre-diabetes (HbA1c 5.7% to 6.4%), and Native Americans have twice the frequency of obtaining DM2 [1-5]. The greatest comorbid disease with DM2 is obesity which affects over 107 million children worldwide [1-5].
Meta-analysis studies of treatments for DM2 have examined how both high intensity, anaerobic exercise and aerobic exercise can effect insulin resistancve [3,4]. However, there is a paucity of research addressing the potential causes of DM2. The purpose of this case report was to discuss changes following food allergen elimination in an obese, Native American patient with Pre-diabetes.
Obesity is comorbid with DM2 and obesity affects approximately 107.7 million children and adolescents worldwide [6- 10]. Therapeutic protocols including diet, exercise, and even pharmacology have been examined as treatments for both obesity and DM2 [6-21]. However, few studies have attempted to examine the contributing causes of DM2 and obesity.
One 12-month study on obesity reduction was completed by Willis et al. (N=94) which used leukocyte reaction tests to identify food allergens for elimination [8]. Those subjects were screened for hypothyroid and hypogonadal secretion anomalies, and each subject chose participation in one of four categories: 1) Food allergen elimination and aerobic-surge exercise, 2) Food allergen elimination alone, 3) Aerobic-surge exercise alone, or 4) Control (only nutritional counseling). All patients received nutritional counseling which taught patients to avoid food with preservatives like high fructose corn syrup, etc. The first two groups were treated with food allergen identification and elimination (ALCAT test of 250 foods, Cell Science Systems, Deerfield Beach, FL, USA).
The greatest changes in that 12-month case/control study were seen in groups treated with food allergy elimination [8]. Other studies have shown significant changes from removing immunologically reactive foods and exchanging processed commercial foods for more natural food choices [8-14]
Case Presentation
This is the first publication of a case where an adolescent was treated for both Prediabetes and obesity by eliminating subacute food allergens. After informed consent was obtained from the 18-year-old patient, a physical examination was performed with body composition testing using bioelectric impedance which showed the fat percentage and total fat mass.
Differential Diagnosis for obesity included hypothyroid secretions, low testosterone, Prader-Willi syndrome, and Idiopathic obesity. Review of patient’s history and recent blood tests of TSH and free testosterone, which eliminated those pathologies from from the diagnosis. The patient’s initial HbA1c level was 6.0% and her BMI was 39.1 (44.4% fat) which yielded a diagnosis of Prediabetes and idiopathic obesity.
Testing for sub-acute food allergens was accomplished using ALCAT leukocyte reactions test (Cell System Labs, Deerfield Beach, FL) which examined reactions from 250 foods, spices and preservatives (Ancho chili peppers to Zucchini squash) [4,20]. Thirty-three (33) foods showed significant reactions, and those foods were eliminated from her diet. The patient was also taught a diff¬erent eating strategy to eat more often (meal or snack every 3 to 4 hours) with appropriate portion sizes (< 2 cups) [8- 12,18,21]. She was also taught how to use the brief, aerobic-surge exercise protocol which increase heart rate with estimated Aerobic- threshold (AT) heart rate formula and maintain this intensity for 2 minutes, 4-5 times each day. The estimated AT Formula used was: (220-age) x 0.75 = target heart rate [12].
Daily tracking of meals/snacks and exercise was completed for the first 30 days with weekly estimates were given for the continuing months in this treatment plan. The patient was seen one month later, with continual follow-ups and testing at 3 and 6 months. The changes seen after the first 90 days were substantial as were the final 6-month results in reduced A1c, BMI, and Fat Mass (Figure 1).
Discussion
While there has been significant work in preventing DM2 [2-5], there has been less research in evaluation of protocols to reduce or reverse the progress of DM2. Food allergen elimination has been examined in reduction of obesity and even irritable bowel syndrome [8-10,16,19,20]. Lewis et al. conducted an immunologic study examining IgG reactions to foods tested to determine if a correlation existed between food allergen elimination and weight loss [10].
Their 90-day study enrolled 120 overweight participants (mean age 45.5, BMI = 29), and eliminating foods that showed increased IgG reactions. Participants, yielded statistically significant changes in body weight (– 5kg, P <0.01) and waist circumference circumference (-5.4cm, P <0.01) [10].
Studies have also discussed food quality and exchanging commercially processed foods for organic foods. Poulsen et al. conducted a randomized, controlled trial which compared an average Danish diet of highly processed foods to a “New Nordic diet” with foods choices higher in fruits, vegetables, fish, and whole grains. That dietary alteration yielded significant changes in fat percentage, waist circumference, and systolic blood pressure for experimental subjects [11].
Processed foods have been correlated with pathologies such as asthma, migraine headaches, irritable bowel syndrome, and studies are now making the connection with obesity [8-12]. Nardocci et al. showed that in Canada, consumption of highly processed foods was correlated with a significantly greater incidence of obesity. Their study showed that “Ultra Processed Foods” made up 45% of the foods consumed by 19,363 adults in this cross-sectional study [13].
There is no question that bariatric surgery is effective in obesity and it has also shown efficacy in DM2 reduction [17]. However, surgery is not a feasible tool in primary care but food allergen testing could be a viable too in primary care. Appropriate intervention is needed for the estimated 107 million children and adolescents who suffer from this growing pathologies of prediabetes, DM2, and obesity [1-21].
In conclusion, this adolescent patient showed substantial reductions in HbA1c% and obesity (BMI and Fat Mass) after food allergen elimination, without pharmaceutical or surgical intervention.
References
1. American Diabetes Association (viewed August 2022). https:// www.diabetes.org/about-us/statistics/cost-diabetes
2. U.S. Center for Disease Control: Type II Diabetes (Viewed April 2022). https://www.cdc.gov/diabetes/basics/type2.html
3. Sampath Kumar A, Maiya AG, Shastry BA, et al. Exercise and insulin resistance in type 2 diabetes mellitus: A systematic review and meta-analysis. Ann Phys Rehabil Med. 2019 Mar;62(2):98- 103. doi: 10.1016/j.rehab.2018.11.001.
4. Nery C, Moraes SRA, Novaes KA, et al. Effectiveness of resistance exercise compared to aerobic exercise without insulin therapy in patients with type 2 diabetes mellitus: a meta-analysis. Braz J Phys Ther. 2017 Nov-Dec;21(6):400-415. doi: 10.1016/j. bjpt.2017.06.004. Epub 2017 Jul 5. PMID: 28728958; PMCID: PMC5693273.
5. Pulgaron ER, Delamater AM. Obesity and type 2 diabetes in children: epidemiology and treatment. Curr Diab Rep. 2014 Aug;14(8):508. doi: 10.1007/s11892-014-0508-y. PMID: 24919749; PMCID: PMC4099943.
6. Center for Disease Control, Obesity Rates (Viewed Aug 2022): http://www.cdc.gov/obesity/data/adult.html
7. Bray GA, Kim KK, Wilding JPH. Obesity: a chronic relapsing progressive disease process: a position statement of the World Obesity Federation. Obes Rev. 2017;18:715-723.
8. Willis FB, Shanmugam R, Southerland JH, et al. Food Allergen Elimination for Obesity Reduction; a Longitudinal, Case-Control Trial. Brit J Gastroenterol. 2020; 2(4): 199-203. doi: 10.31488/ bjg.1000122 https://britishjournalofgastroenterology.com/ food-allergen-elimination-for-obesity
9. Willis FB, Shanmugam R, Curran, SA. Food Allergen Eliminations and Combined Protocols for Obesity Reduction: a Preliminary Comparison Study. Food Sci Nutrition Res. 2018; 1(1):1-3.
10. Lewis JE, Woolger JM, Melillo A, et al. Eliminating immunologically- reactive foods from the diet and its effect on body composition and quality of life in overweight persons. J Obes Weig loss Ther. 2012: 2(1):1-6.
11. Poulsen SK, Due A, Jordy AB, et al. Health effect of the New Nordic Diet in adults with increased waist circumference: a 6-mo randomized controlled trial. Am J Clin Nutr. 2014; 99(1):35-45.
12. Willis FB, Curran S. Brief, Aerobic-surge Exercises for Effective Weight Loss: a Randomized, Controlled Trial. Med Clin Res. 2019; 4(11):1-5
13. Nardocci M, Leclerc BS, Louzada ML, et al. Consumption of ultra-processed foods and obesity in Canada. Can J Public Health. 2019 Feb;110(1):4-14. doi: 10.17269/s41997-018-0130-x.
14. Willis FB, Brackman SM. Food is the Cause and the Cure for the Obesity Epidemic. Medical Clinical Research. 2020:5(1):1-3.
15. Kelly AS, Auerbach P, Barrientos-Perez M, et al. A Randomized, Controlled Trial of Liraglutide for Adolescents with Obesity. N Engl J Med. 2020 May 28;382(22):2117-2128.
16. Zouras S, Stephens JW, Price D. Obesity-related hypogonadism: a reversible condition. BMJ Case Rep. 2017. doi: 10.1136/bcr- 2017-220416
17. Sheng B, Truong K, Spitler H, et al. The Long-Term Effects of Bariatric Surgery on Type 2 Diabetes Remission, Microvascular and Macrovascular Complications, and Mortality: a Systematic Review and Meta-Analysis. Obes Surg. 2017 Oct;27(10):2724- 2732. doi: 10.1007/s11695-017-2866-4. PMID: 28801703.
18. Iwao S, Mori K, Sato Y. Effects of meal frequency on body composition during weight control in boxers. Scand J Med Sci Sports.1996; 6: 265-72.
19. Hostalek U, Campbell I. Metformin for diabetes prevention: update of the evidence base. Curr Med Res Opin. 2021 Oct;37(10):1705- 1717. doi: 10.1080/03007995.2021.1955667. Epub 2021 Jul 28. PMID: 34281467.
20. Ali A, Weiss TR, McKee D, et al. Efficacy of individualised diets in patients with irritable bowel syndrome: a randomised controlled trial. BMJ Open Gastroenterol, 2017 Sep 20;4(1):e000164. doi: 10.1136/bmjgast-2017-000164.
21. Willis FB. Food is the Cure for the Overweight Disease. Galveston Press (Texas, USA, 2020), p 13-37.
Received: May 16, 2022;
Accepted: May 30, 2022;
Published: May 31, 2022.
To cite this article : Buck Willis F, Arogundade R, Teimouri E, et al. Prospective Evaluation of Predictive Indexes for Esophageal Varices in Children and Adolescents with Portal Hypertension. British Journal of Gastroenterology. 2022; 4(2): 254-256. doi: 10.31488/bjg.1000131.
© Buck Willis F, et al. 2022.
