Review Article / Open Access
DOI: 10.31488/bjg.1000122
Food Allergen Elimination for Obesity Reduction; a Longitudinal, Case-Control Trial
F. Buck Willis*1, Ram Shanmugam*2, Janet H. Southerland*3, Charles P. Mouton*4
1. Galveston ClinicalResearch,Corresponding Author: 6341 Stewart Rd #115, Galveston TX 77551, USA
2. Texas State University, School of HealthAdministration, USA
3. University of Texas Medical Branch,Galveston, USA
* Corresponding author: Galveston ClinicalResearch, 6341 Stewart Rd #115, Galveston TX 77551, USA, Tel: 1-409-632-7131
Abstract
Objectives: This study was designed to examine efficacy of separate and combined protocols for obesity reduction with sequential outcomes after one year. This was an experimental case vs control study, lasting 12 months, conducted from 2018 to 2020.Methods: Ninety-four obese subjects, ages 14-76 with Body Mass Index (BMI) > 30, enrolled in this multi-center study in Texas, USA. Treatments included food allergen identification/elimination (ALCAT, leukocyte reaction test which showed reactions to 237 foods) and/or a brief, aerobic-surge exercise (2-minute sessions, 5/day). Foods with significant reaction for each subject were eliminated from their diet for 12 months (mean 36 foods/subject).Subject categorization was as follows: Group 1 Combined Food Allergen Elimination and Aerobic-surge exercise (N=23); Group 2 Food Allergen Elimination alone (N=23); Group 3 Aerobic-surge exercise alone (N=18); Group 4 was the Control group who chose no treatments (N=30). The dependent variables included changes in weight, BMI, and waistcircumference.Results: There was a significant difference between groups and between therapeutic protocols (P < 0.0001). The greatest changes came from Group I, Combined (Mean changes: Weight -32.2lbs, BMI -4.6, and Waist -4.3 inches). Subjects who chose food allergen elimination alone, also showed a significant change in comparison to exercise-only and control subjects (P < 0.0001).Conclusion: Food allergen elimination was effective for obesity reduction in this 12- month study.
Keywords: Weight Loss, aerobic-surge, ALCAT testing
Introduction
Examining effective treatments for obesity is imperative because now over 155 million adults in the USA, UK, and Australia are estimated to be categorically obese (BMI > 30) [1-6]. This is also financially important because the US Center for Disease Control has estimated that obesity costs an additional $1400/year in greater health care expenses for each obese person [1,3,6]. An important question remains what are the best approaches to address the underlying causes of obesity that may or may not be genetically driven.
While many different methods for treating obesity have been examined [3-22], there is only a paucity of data in studies that have tried to identify and counteract the specific causes of the obesity disease [3,6,8]. Studies have examined efficacy of performing therapeutic exercises,[11-14], eating organic or natural foods [15-19], and even portion size control for obesity reduction [20-22]. Leukocyte testing has been used for treating other diseases such as Irritable Bowel Syndrome (IBS) [23,24,27] and migraine headaches [25,26]. However, only one comparison pilot study examined leukocyte reactions for obesity reduction (ALCAT test, Cell Science Systems, Deerfield beach, FL) [3].
In that study, food allergen testing for elimination of allergens (leukocyte reaction tests to 237 foods) was used for all subjects (N=17) and in that study 10 subjects also employed the aerobic-surge exercise bouts (4.3/day) with the practice of eating more often (5 times/day) in smaller portion sizes (< 2 cups/meal or snack). Even with this small sample size, there were statistically significant changes in weight, body fat percentage, and BMI for all participants(p< 0.0001). There was also a significant difference between groups (ALCAT only vs ALCAT plus combined protocols, p < 0.001). A 12-month follow up analysis of that study showedfinancial savings of $1900/year in reduced medical expenses after patients became less obese and achieved a BMI < 26.
Brief, high intensity exercise has become a novel protocol in weight loss and a recent randomized controlled trial was conducted on the brief, 2-minute aerobic-surge exercise method [11]. Willis and Curran enrolled 46 obese subjects (mean BMI = 32.6, mean age 39±2) and the Experimental group subjects were taught how to use 40 different exercises, to reach a heart rate (HR) within the estimated aerobic threshold (220-age) x 0.75. This exercise was then maintained (at elevated HR) for 2 minutes. Control subjects were simply told “Exercise more” which is often the direction given in primary care and control subjects were not taught the Aerobic-threshold training. No dietary changes were made for either group.
The variables examined in that study included change in Weight, ‘Body summation’ of 10 girth measurements, and change in BMI in this 60-day study at three sites. There was a significant difference between groups (p < 0.0001, T=2.699). The Experimental group averaged completing 4.2 of the 2-minute, Aerobic-surge exercise bouts daily, and their changes were as follows: -8.2kg (±3.0), -47.5cm girth sum (±15), and -3.3 BMI (±0.2). The Control groups mean changes were: +0.6kg (±1kg), +4.3cm girth sum (±4.0), and +0.2 BMI (±0.2). This study showed efficacy of the brief, high intensity exercise but without long term outcomes[11].
A paper by Willis and Brackman, “Food is the Cause and the Cure for the Obesity Epidemic” compared research of leukocyte reaction testing and organic foods in weight loss [6]. They discussed significant changes from simply exchanging processed foods for natural foods and even how eating single portion sizes (2 cup servings) was also effective in weight loss.That review also discussed that an estimated 21% of the US population has significant, acute food allergies [4] and reduction of foods allergens has also showed significant changes inotherpathologies [23-27]. Sub-acute food allergies has been hypothesized as a potential contributing cause of the obesity disease and epidemic [5-9,23].
The purpose of this study was to examine separate and combined efficacy of food allergen testing/elimination and/or aerobic-surge exercise bouts with longitudinal outcomes.
Methods
Ninety-four participants (mean age 53.4, range 14-76) were enrolled after qualifying with BMI greater than 30 kg/m2. The treatment methods included food allergen identification/elimination and/or brief, aerobic-surge exercise bouts (2-minutes, 5/day), or control. The dependent variables included changes in weight, BMI, and waist circumference.The independent variables were age and gender (Table 1).
Table 1. Demographics
| Groups | Total | Male | Female | |
|---|---|---|---|---|
| Group 1. | Food Allergen Elimination and Exercise | 23 | 9 | 14 |
| Group 2. | Food Allergen Elimination only | 23 | 8 | 15 |
| Group 3. | Exercise only | 18 | 8 | 10 |
| Group4. | Control | 30 | 6 | 24 |
| Subjects Enrolled | 94 | 31 | 63 |
After written informed consent, these participants were given the choice of which separate or combined treatment methods they wished to employ. Participants choosing food allergen elimination (combined category or separate) (N=46) were tested using the ALCAT, Leukocyte reaction test showing reactions to 237 foods. Foods with significant reaction (categorically acute or moderate reactions) were eliminated for this study (mean 36 foods).
Participants who chose to be treated with the aerobic-surge exercise (combined category or separate) (N=41 total) were taught how to use 40 different exercises to raise their Heart Rate (HR) to 75% of each subject’s maximum HR for two minutes. The estimated aerobic-thresholdis (220-age) x .75 and this HR was maintained for only 2-minutes, 4-5 times/day. They were taught how to use example exercises of scissor kicks or dumb-bell curls to achieve the calculated aerobic threshold and Heart Rate as shown with a finger-tip pulse monitor. (Daily tracking was reported to the coordinator by eachsubject.)
We performed an unmatched, case-control study on our participants comparing those who chose any of the treatment approaches to those who chose none of the treatment approaches (control). This study was approved by the Galveston Clinical Research Foundation IRB (Approval number 2018.0218)). Using frequency distribution and Analysis of Variance methods, we analyzed the associations with each of our treatment methods with each of our dependent variables. The analysis was performed with SPSS software.
Results
There was a total of 92 participants who completed this study. Group 1, consisted of subjects who chose both Combined Food Allergen Elimination and Aerobic-surge exercise (N=23); Group 2 used Food Allergen Elimination alone (N=23): Group 3 chose Aerobic-surge exercise alone (N=16); Group 4 was the Control group who chose no treatments (N=30). The variable analyzed was the weight loss (Figures 1 and 2). Their sample average weight loss, standard deviation, and the 95% confidence interval (CI) are displayed in Table 2 below. The Group 2 is more heterogeneous than any other group. The 95% CI are indicative of their overlapping possible weight losses.
Table 2. Summary of the group's performances
| Group | Average Weight | Standard | 95% CI | |
|---|---|---|---|---|
| Loss (pounds) | Deviation | Lower | Upper | |
| Combined Food Allergen Elimination and Aerobic-surge Exercise | -32.21 | 9.41 | -36.28 | -28.14 |
| Food Allergen Elimination alone | -26.08 | 12.62 | -31.54 | -20.62 |
| Aerobic-surge exercise alone | -14.12 | 4.36 | -16.45 | -11.79 |
| Control | -2.96 | 6.03 | -5.22 | -0.71 |
The standardized weight loss was normally distributed, according to the probability- probability (P-P) plot. The Normality is essential for all statistical analyses. Clearly, the Figure 1 implies that the Group 1 performed much superiorly on the average, followed by the Group 2,the Group 3, and Group 4. Interestingly, their differences are equallyspaced.
The same meaning is echoed in Figure1 with a knowledge that there were unusuall yover-achieving performances by the participant swith identifiers(ID)42and 44 in Group2,68 in Group 4 and none in Group 1 and in Group 3. Likewise, the unusually under-achieving performancesby the participants with identifiers (ID) 40 in Group2 and 66 in Group 4 while none in Group 1 and in Group3.However, in an over-all sense, the four groups significantly differ from each otheraccording to the F-value,F(3df ,88df )=56.86 at a significance level less than 0.0001. In other words,the null hypothesis H0:µ1=µ2=µ3=µ4is rejected at aconfidence leve l1 -α=99.91% in favor of there search hypothes is H1:at_least_two_groups_differ_siginificantly,where µ1, µ2, µ3, µ4 denote respectively the population average weight loss of future participants in the Groups1,2,3,and 4.Now,the questionis what group is significantly different from which group. To answer this question.
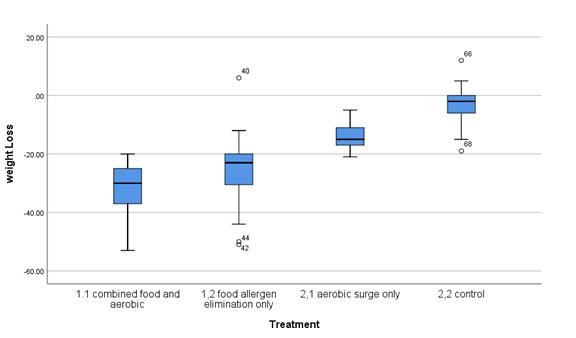
Figure 1. Weight loss with outliers
A multiple comparison analysis was performed, and the data analytic results indicate the followingin asequential manner.The Group1 differs from the Group2, Group3,and Group4 at a significance leve l0.02,lessthan0.0001,and less than 0.0001, respectively .The Group2 differs from the Group 3, and Group 4 at a significance level less than 0.0001, and less than 0.0001, respectively. The Group 2 differs from the Group 3, and Group 4 at a significance level less than 0.0001,and lessthan0.0001,respectively.The Group3 differs from the Group4 at a significance level less than0.0001.
Discussion
Obesity is now described as a “disease” [28,29,32] and the WHO describes it as a “chronic relapsing disease process” with food as the “primary agent” [29]. It has been hypothesized that sub-acute food allergens are a significant contributing factor in obesity [3,5,8], and this current study investigated the contributing role of elimination of food allergens to weight control. Our results confirm previous research demonstrating that participants who had food allergen testing and elimination in this study showed a significant change in comparison to all other subjects (N < 0.0001).
Lewis et al. conducted a study examining IgG reactions to foods and showed a direct correlation with changes in only 90 days [8]. They enrolled 120 overweight participants (mean age 45.5, BMI = 29), eliminated foods positive for increased IgG levels, reactions. Participants showed significant improvement in Weight (– 5kg, P<0.01) and Waist circumference (-5.4cm, P<0.01). The study did not test for other Immunoglobulin reactions (IgE, IgM, etc.) nor did they test obese subjects, but it did show a statistically significant change of food allergen testing and elimination after only 90 days [8].
Similarly, findings in that study also showed that eliminating food allergens combined with increasing aerobic activity has a synergistic effect on weight control and obesitymanagement. It confirms previous pilot work by Willis et al showed that the combination of food allergen elimination and aerobic-surge exercise yielded statistically significant changes in weight, body fat percentage, and BMI [3].
Strengths and limitations
Food allergen elimination from ALCAT test results (Cell Science Systems laboratories) showed a significant difference in all variables for 12 months (p < 0.0001). However, this is a case-control study and not a randomized control trial.
Therefore, direct correlations and inference about treatment may be influenced confounding. Second, this study has a relatively small sample size compared to other studies focused on weight control and obesity.
Despite this issue, we were still able to demonstrate statistically significant difference between interventions. Finally, the study period was relatively short and it is unclear if our participants will show evidence of long durations of weight control. However, our follow-up of study participants is similar to many other studies of weight control and obesity.
The World Health Organization considers obesity to be a global epidemic, effecting over 650 million adults who are obese [2] and over 2.0 billion adults who are overweight (BMI >26- 30) [28-33].
The purpose of this study was to examine separate and combined efficacy of food allergen testing/elimination and/or aerobic-surge exercise bouts with longitudinal outcomes. The changes were significant (p < 0.0001) and while the exercise was beneficial, this is the first study to show food allergens as a contributing factor in obesity with longitudinal outcomes (Figure 2). Future studies should examine both immediate evidence from foodallergen testing/elimination (90 days) with longer durations (36 months) and more variables (body composition testing) to measure pure efficacy of this combined approach addressing obesity.
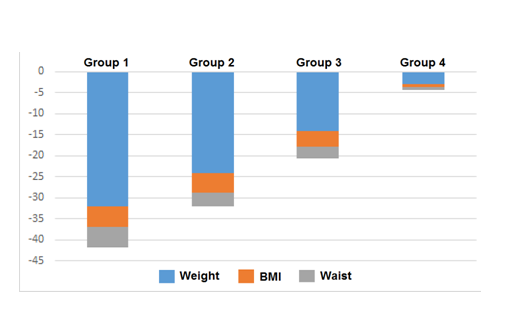
Figure 2. Stacked Changes after 12-months
Conclusion
Our study confirms that eliminating food allergens and performing aerobic-surge exercise was effective in changing the dependent variables for both male and female subjects. Both the polarity and proximity of the age and gender shift differently from each other’s with respect to the standardized body weight (pounds), BMI (kg/m2), and waist circumference (inches).
Acknowledgement
Authors would like to thank Nicole Maul MS and Sheri Brackman MS for their insight and editing. The results of the study are presented clearly, honestly, and without fabrication, falsification, or inappropriate data manipulation.
Conflict of Interest
None of the authors have conflict of interest in this study.
Funding
This study was completed without extramural funding.
Ethical Statement
The article was not plagiarized and had not previously been published in other journals.
References
1. Center for Disease Control, Obesity rates. http://www.cdc.gov/obesity/data/adult.html
2. WHO Obesity (viewed 2020) https://www.who.int/news-room/fact-sheets/detail/obesity- and-overweight
3. Willis FB, Shanmugam R, Curran, SA. Food Allergen Eliminations and Combined Protocols for Obesity Reduction: a Preliminary Comparison Study. Food Sci Nutrition Res.2018; 1(1):1-3.
4. Chen J. Making a Case for Food Sensitivity Testing, Huffington Post (viewed November 2017) https://www.huffingtonpost.com/julie-chen-md/making-a-case-for-food- se_b_8387196.html
5. Deutsch RD, Rivera R. Your Hidden Food Allergies Are Making You Fat. Prima Press, (CA). 2002;62-84.
6. Willis FB, Brackman SM. Food is the Cause and the Cure for the ObesityEpidemic. Medical Clinical Research. 2020:5(1):1-3.
7. “Food Intolerance and Sensitivity,” British Allergy Foundation.https://www.allergyuk.org/information-and-advice/conditions-and-symptoms/36-food-allergy
8. Lewis JE, Woolger JM, Melillo A, et al. Eliminating immunologically-reactive foods from the diet and its effect on body composition and quality of life in overweightpersons. J ObesWeig loss Ther 2012: 2(1):1-6.
9. “Food Allergy Basics: Facts and Statistics,” Food Allergy Research andEducation, https://www.foodallergy.org/facts-and-stats
10. Luo X, Xiang J, Dong X, et al. Association between obesity and atopic disorders in Chinese adults: an individually matched case-control study. BMC Public Health. 2013;13:12
11. Willis FB, Curran S. Brief, Aerobic-surge Exercises for Effective Weight Loss: a Randomized, Controlled Trial. MedClinRes.2019; 4(11):1-5
12. Blair SN, Church, TS. The fitness, obesity, and health equation: is physicalactivity the common denominator? JAMA. 2004;292(10):1232-4.
13. Daley AJ, Copeland RJ, WrightNP, et al. Exercise therapy asa treatment for psychopathologic conditions in obese and morbidly obese adolescents: a randomized, controlled trial. Pediatrics. 2006;118(5):2126-34.
14. Jakicic JM, Otto AD. Treatment and prevention of obesity: what is the role of exercise? Nutr Rev. 2006;64(2 Pt2):S57-61.
15. Poulsen SK, Due A, Jordy AB, et al. Health effect of the New Nordic Diet in adults with increased waist circumference: a 6-mo randomized controlled trial. Am J Clin Nutr. 2014;99(1):35-45.
16. Palmer DJ, Huang RC,Craig JM, Prescott SL. Nutritional influences onepigenetic programming: asthma, allergy, and obesity. Immunol Allergy Clin North Am. 2014 Nov;34(4):825-37.
17. Fries WC. The Natural Diet: Best Foods for Weight Loss. 2017https://www.webmd.com/diet/features/the-natural-diet-best-foods-for-weight-loss#1 t.
18. Hurtado-Barroso S, Tresserra-Rimbau A, Vallverdú-Queralt A, et al. Organic food and the impact on human health. Crit Rev Food Sci Nutr. 2017; 30:1- 11.
19. Pergola G, Foroni F, Mengotti P, et al. A neural signature of food semantics is associated with body-mass index. Biol Psychol. 2017; 129:282-92.
20. Torbahn G, Gellhaus I, Koch B, et al. Reduction of Portion Size and Eating Rate Is Associated with BMI-SDS Reduction in Overweight and Obese Children and Adolescents: Results on Eating and Nutrition Behaviour from the ObservationalKgAS Study. Obes Facts. 2017; 10:503-16.
21. Kesman RL, Ebbert JO, Harris KI, et al. Portion control for the treatment of obesity inthe primary care setting. BMC Res Notes. 2011;4:346.
22. Iwao S, Mori K, Sato Y. Effects of meal frequency on body composition duringweight control in boxers. Scand J Med Sci Sports.1996; 6:265-72.
23. Ali A, Weiss TR, McKee D, et al. Efficacy of randomized diets in patients with irritable bowel syndrome: a randomized controlled trial. BMJ Open Gastroenterol. 2017; 20: e000164.
24. Atkinson W. Food elimination based on IgG antibodies in irritable bowel syndrome:a randomised controlled trial. Gut.2004;53(10):1459-64.
25. Alpay K, Ertaş M, Orhan EK, et al. Diet restriction in migraine, based on IgG against foods: A clinical double-blind, randomized, cross-over trial. Cephalalgia . 2010;30(7):829-37.
26. Arroyave Hernández CM, Echavarría Pinto M, Hernández Montiel HL. Food allergy mediated by IgG antibodies associated with migraine in adults. Rev Alerg Mex. 2007;54(5):162-8.
27. Hungin A, Chang L, Locke G, et al. Irritable bowel syndrome in the United States: prevalence, symptom patterns and impact. Alimentary Pharmacology and Therapeutics.2005;21(11):1365-1375.
28. Wilding JPH, Mooney V, Pile R. Should obesity be recognised as a disease? BMJ. 2019;366:l4258.
29. Bray GA,Kim KK,Wilding JPH. World Obesity Federation. Obesity: a chronic relapsing progressive disease process. A position statement of the World Obesity Federation. Obes Rev. 2017;18(7):715-23.
30. Sicherer SH,Sampson HA. Food allergy: Epidemiology, pathogenesis, diagnosis,and treatment. J Allergy Clin Immunol. 2014;133(2):291-307.
31. Bhat SP, Sharma A. Current Drug Targets in Obesity Pharmacotherapy – AReview. Curr Drug Targets. 2017;18(8):983-93.
32. Willis FB. Food is the Cure for the Overweight Disease. Galveston Press (TX):2019; 13-37.
33. Xiumei Ma,Qing Chen, et al. Skipping breakfast is associated with overweight and obesity: A systematic review and meta-analysis. Obes Res Clin Pract. 2020;14(1):1-8.
Received: August 05, 2020;
Accepted: August 12, 2020;
Published: August 19, 2020.
To cite this article : Willis FB, Shanmugam R, Janet H, et al. Food Allergen Elimination for Obesity Reduction; a Longitudinal, Case-Control Trial. British Journal of Gastroenterology. 2020; 2:4.
©Willis FB, et al.2020.
